How does cataract surgery work?
- primevisionarkan@gmail.com
- Arkan Medical Building 7, Fifth floor Clinic C5-1
- 01080677020
10:00AM - 10:00PM
- All Services
- LASIK SURGERIES
- CORNEAL TRANSPLANT
- CATARACT SURGERIES
- GLAUCOMA SURGERIES
- VITREO - RETINAL SURGERIES
- --Vitrectomy
- --INTRA- VITREAL INJECTIONS
- PEDIATRIC SURGERY
- --Strabismus
- --Congenital Cataract
- --Congenital Glaucoma
- OCULOPLASTIC SURGERIES
- --Eyelid surgery
- --DCR
- --Orbital Surgeries
- EYE MEDICAL DISEASES
- CONTACT LENSES
A cataract is the clouding of the natural intraocular crystalline lens, which focuses light onto the retina. This cloudiness can decrease vision and, if left untreated, may lead to blindness. Cataracts typically develop slowly and painlessly, causing gradual vision changes that may not be immediately noticeable. Worldwide, cataracts are the leading cause of preventable blindness. Currently, there are no medical treatments to prevent the development or progression of cataracts. The only definitive treatment is modern cataract surgery, which involves removing the cloudy lens and implanting a clear intraocular lens (IOL). Cataract surgery is one of the most effective and commonly performed medical procedures, with an overall success rate of 97 percent or higher in appropriate settings.
Cataracts often cause a gradual decline in vision that glasses cannot correct. Common symptoms include blurry vision, difficulty reading in dim light, poor night vision, glare and halos around lights, and occasionally double vision. Frequent changes in glasses prescriptions and a new ability to read without reading glasses in individuals over 55 can also indicate cataracts.
Cataracts can be categorized into several types: age-related, traumatic, and metabolic. Age-related cataracts are the most common and have a multifactorial pathogenesis that is not fully understood. Traumatic cataracts can develop from blunt or penetrating eye injuries, electrocution, chemical burns, or radiation exposure. Metabolic cataracts occur in conditions such as uncontrolled diabetes, galactosemia, Wilson disease, and myotonic dystrophy.
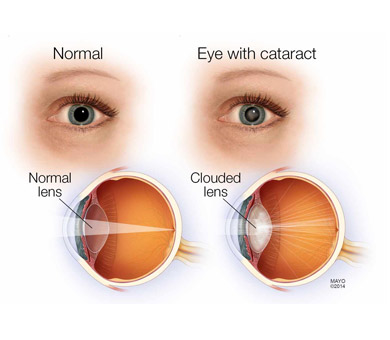
Vision Problems with Cataracts
- Blurred Vision: Difficulty seeing clearly at a distance or near; different types may affect either distance or near vision more.
- Glare: Halos or streaks around lights, and difficulty seeing in bright light.
- Double Vision: Seeing a double or a ghosted image in the eye with a cataract.
- Night Vision Issues: Trouble seeing well at night or needing more light to read.
- Loss of Contrast Sensitivity: Reduced ability to distinguish between different shades and contrasts.
- Color Perception Changes: Colors may appear faded or yellowed.
- Light Sensitivity: Increased sensitivity to light, particularly from oncoming headlights at night.
- Increasing Near-Sightedness: Changes in refractive status, including the “second sight” phenomenon where near vision temporarily improves.
If you experience any of these symptoms, consult your ophthalmologist.
Risk Factors for Cataract Development
- Diabetes or Elevated Blood Sugar
- Steroid Use (oral, IV, or inhaled)
- Ultraviolet Exposure
- Smoking
- Ocular Diseases: Retinitis Pigmentosa, Uveitis
- Ocular Trauma
- Prior Ocular Surgery
- Genetic Predisposition
- Cataracts Associated with Dermatologic Diseases
- Radiation or Chemotherapy
Common Types of Cataracts
- Age-Related Cataracts: The most common type, divided into three anatomical categories:
- Nuclear Sclerotic Cataracts
- Cortical Cataracts
- Posterior Subcapsular Cataracts
Patients may develop opacities in multiple areas of the lens, leading to overlap in classification.
Ophthalmic Examination
- Visual Function Assessment: Includes evaluating how vision affects daily activities and measuring visual acuity with and without glasses. Glare testing involves reading an eye chart under bright light or using instruments to simulate glare.
- Comprehensive Dilated Eye Exam: Assesses cataract severity, pupil size, corneal clarity, and health, lens stability, anterior chamber depth, and optic nerve and retina health.
Preoperative Measurements
To achieve optimal visual outcomes, several measurements are taken:
- Refraction: Ensures consistent vision correction between eyes if only one eye is operated on.
- IOL Power Determination: Measures axial length, corneal refractive power, and anterior chamber depth. Additional tests like corneal topography and endothelial cell counts may be used in certain cases.
Cataract Surgery
- Indication for Surgery: Cataract removal is only necessary if symptoms significantly impair daily activities. If cataracts are not affecting your life, a new eyeglass prescription might suffice.
- Surgical Procedure: Cataract surgery involves removing the cloudy lens and replacing it with a clear intraocular lens (IOL). This is typically performed as an outpatient procedure, and the choice of IOL is based on individual visual needs.
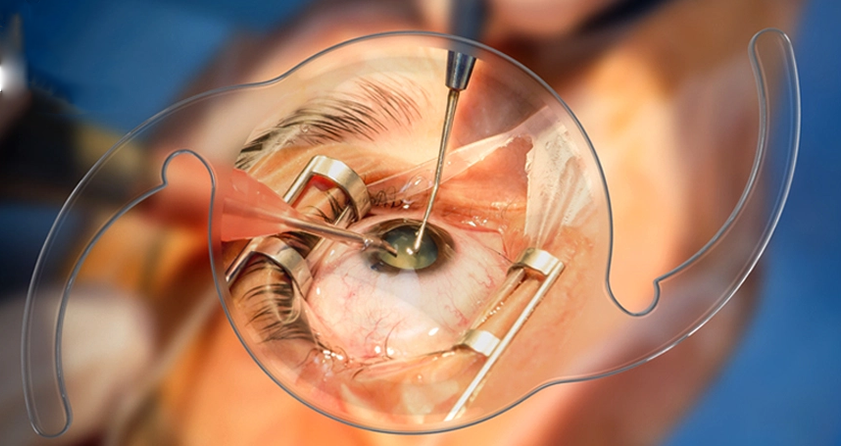
During Cataract Surgery
Your eye surgeon will remove the cloudy natural lens from your eye and replace it with an artificial lens called an intraocular lens (IOL). Before your cataract surgery, your doctor will discuss the different types of IOLs and how they work.
In some cases, people may experience hazy vision years after cataract surgery due to cloudiness in the lens capsule, which holds the IOL in place. If this happens, your ophthalmologist can use a laser to open the cloudy capsule and restore clear vision. This procedure is called a laser posterior capsulotomy.
Cataracts are a common cause of vision loss, but they can be effectively treated. You and your ophthalmologist should discuss your cataract symptoms and decide if cataract surgery is right for you.
What to Expect with Cataract Surgery
Before Surgery:
- Eye Measurements: Your surgeon will measure your eye to determine the proper focusing power for your IOL. This test is called biometry.
- Medication Review: Inform your doctor about any medications you are taking. You might be advised to stop certain medications before surgery.
- Eye Drops: You may be prescribed eye drops to use before surgery. These drops help prevent infection and reduce swelling during and after the procedure.
- Phacoemulsification: This is the most common method for removing the cataract. It uses ultrasound to break up the cloudy lens into small pieces, which are then suctioned out. The natural lens is usually replaced with an IOL.
The Day of Surgery:
- Pre-Surgery Instructions: Your ophthalmologist may ask you not to eat solid food for at least 6 hours before surgery.
- Surgery Location: Cataract removal surgery can be performed in an outpatient surgery center or a hospital.
During Surgery:
- Procedure: The surgery typically takes about 10 minutes. An ultrasound instrument will break up the cloudy lens into small pieces, which are then suctioned out.
- Anesthesia: Your eye will be numbed with eye drops or an injection around the eye. You may also receive medication to help you relax.
- Awareness: You will be awake during the surgery. You may see light and movement but won’t see what the surgeon is doing.
- Surgical Technique: Your surgeon will use a special microscope to create tiny incisions with a micro-blade around the edge of your cornea. The cataract will be broken up and removed, and the new IOL will be implanted.
- Incisions: Usually, no stitches are needed as the incisions are self-sealing and will close on their own. A shield will be placed over your eye to protect it while you heal.
- Recovery: You will rest in a recovery area for about 18 to 30 minutes before being ready to go home.
How Long Does It Take to Recover from Cataract Surgery?
A Few Days After Surgery:
- Eye Drops: You may need to use eye drops as prescribed. Follow your doctor’s instructions carefully.
- Avoid Irritants: Keep soap and water out of your eye. Do not rub or press on your eye.
- Protective Measures: You may be advised to wear eyeglasses or a shield to protect your eye, especially when sleeping.
- Activity Restrictions: Your ophthalmologist will guide you on when you can safely resume activities like exercising and driving.
